The Effect of Pseudomonas Infection with Burns Patients
Abstract
Pseudomonas aerginosa is Gram-negative, facultative aerobic rods, non- fermentative, non-sporulation, motile by polar flagellum one and the most important and opportunistic pathogens that cause a high rate of mortality and morbidity in hospitalized patients with compromised immune systems. It has the ability to infect almost all tissues of the body as a result of its possession of a large variety of virulence factors that contribute significantly to the pathogenicity of the host, so the rapid detection of these bacteria plays a crucial role in controlling the diseases that cause them, especially in burn injuries. More than 120 samples were collected, clinical samples for people with burns of both the second and third degree, were collected from the burn unit at Imam Al-Sadiq Hospital (peace be upon him) in Babylon, during the period from November 2022 to January 2023, to investigate the spread of P. aeruginosa bacteria that these bacteria have it with age from (1year to above 61year) , 57male, 63 female. The growing isolates were diagnosed after their cultivation on Blood agar and MacConkey agar by selective medium, Pseudomonas chromogenic agar, and the diagnosis was confirmed using the vitek2 compact system, aeruginosa isolates. The results of the current study, which included information about patients with burns such as gender, age, type of burn and degree of burn, showed that the number of diagnosed cases as burn injuries for males was 47.5%, while the percentage of females was 52.5%. The highest rate of infection was in the age group 1-10 years at 35%, which is the category of children, followed by the age group 11-20 with 23.3%, and the lowest infection rate was in the age group 51-60 and the group above 61 with 1.7%.Thus,there were a high significant difference (P ≤ 0001). The results indicated that the diagnosed cases of injuries were distributed in varying proportions with regard to the type of burn, as the highest percentage of burn injuries was from liquid burns by 50%, followed by burns by fire at 46.7%, and the lowest percentage of injuries was for electric shock burns by 3.3%.Thus, there was a significant difference (P ≤ 0.002). The results of the study showed that the highest percentage was for P. aeruginosa, 68(68%), Klebsiella 12(12%), Eschreichia coli 10(10%), Proteus 4(4%), and the least was Acinetobacter and Citrobacter 3(3%). This study concluded that the prevalence of P. aeruginosa bacteria is high among clinical samples.
Full text article
References
Mahon, C. R., Lehman, D. C., & Manuselis, G. (2018). Textbook of diagnostic microbiologye-book. Elsevier Health Sciences.
MacFaddin, J. F. (2000). Biochemical tests for the identification of medical bacteria. 3rd Ed. The Williams and Wilkins- Baltimor, USA
Wanger, A., Chavez, V., Huang, R., Wahed, A., Dasgupta, A., & Actor, J. K. (2017). Microbiology and molecular diagnosis in pathology: a comprehensive review for board preparation, certification and clinical practice.
Levinson, W. (2016). Review of Medical Microbiology and Immunology. 14thed.McGraw-Hill education, Inc. PP 821.
Hemraj, V.; Diksha, S. and Avneet, G. (2013). A Review on Commonly Used Biochemical Test for Bacteria. IJLS. 1(1): 1-7.
Fritsche, T.R. ; Swoboda, S.E.; Olson, B.J.; Moore, F.M.; Meece, J.K. and Novicki, T.J. (2011) . Evaluation of The Sensititre ARIS2x and Vitek 2 Automated Systems for Identification of Bacteral Pathogens Recovered from Veterinary Specimens. Marshfield labs. LACROSSE. University of Wisconsin
Jawetz, E., Melnik, J.L. ; Adelberg , E.A.; Brook, G.F.; Butel, J.S. and Morse ,S.A. (2008). Medical Microbiology 26th. ed. Appleten and Lang New York Connctical. PP.45-60 .
W. S. Hsieh, L. L. Sung, K. C. Tsai and H. T. Ho, APMIS, 2009
M. J. Bruins, P. Bloembergen, G. J. H. M. Ruijs and M. J. H. M. Wolfhagen, J. Clin. Microbiol., 2004
Driscoll, J. A., Brody, S. L., & Kollef, M. H. (2007). The epidemiology, pathogenesis and treatment of Pseudomonas aeruginosa infections. Drugs, 67, 351–368. https://doi.org/10.2165/00003495-200767030-00003
Moghaddam, M. M., Abolhassani, F., Babavalian, H., Mirnejad, R., Barjini, K. A., & Amani, J. (2012). Comparison of in vitro antibacterial activities of two cationic peptides CM15 and CM11 against five pathogenic bacteria: Pseudomonas aeruginosa, Staphylococcus aureus, Vibrio cholerae, Acinetobacter baumannii, and Escherichia coli. Probiotics and Antimicrobial Proteins, 4(2), 133–139. https://doi.org/10.1007/s12602-012-9098-7
Riou, M., Carbonnelle, S., Avrain, L., Mesaros, N., Pirnay, J. P., Bilocq, F., Glupczynski, Y. (2010). In vivo development of antimicrobial resistance in Pseudomonas aeruginosa strains isolated from the lower respiratory tract of Intensive Care Unit patients with nosocomial pneumonia and receiving antipseudomonal therapy. International Journal of Antimicrobial Agents, 36(6), 513–522. https://doi.org/10.1016/j.ijantimicag.2010.08.005
Deschaght, P., Van daele, S., De Baets, F., & Vaneechoutte, M. (2011). PCR and the detection of Pseudomonas aeruginosa in respiratory samples of CF patients. A literature review. Journal of Cystic Fibrosis. https://doi.org/10.1016/j.jcf.2011.05.004
Gerasimova, Y. V., & Kolpashchikov, D. M. (2013). Folding of 16S rRNA in a signal-producing structure for the detection of bacteria. Angewandte Chemie - International Edition, 52(40), 10586–10588. https://doi.org/10.1002/anie.201303919
Pereima, M.J.L., Leal, M., Capella, M.R., Goldberg, P., Quaresma, E.R., Araújo, E.J. and Souza, J.A. 2001. Análise de 573 crianças com queimaduras internadas no Hospital Infantil Joana de Gusmão. Rev Bras Queimaduras, 1 (1), pp.41-48.
Peranantham, Manigandan, G. and Shanmugam, K., 2014. Forensic approach to a case of death due to burn injury: a case report. International Journal of Research in Medical Sciences, 2 (3), p.1214-6.
Gnaneswaran, N., Perera, E., Perera, M. and Sawhney, R. 2015. Cutaneous chemical burns: Assessment and early management. Australian Family Physician, 44 (3), pp.135-139.
Lloyd, E.C.O., Rodgers, B.C., Michener, M. and Williams, M.S. 2012. Outpatient burns: Prevention and care. American Family Physician, 85 (1), pp.25-32.
Toussaint, J. and Singer, A.J. 2014. The evaluation and management of thermal injuries: 2014 update. Clinical and Experimental Emergency Medicine, 1 (1), pp.8-18.
Fariñas, M. C., & Martínez-Martínez, L. (2013). [Multiresistant Gram-negative bacterial infections: Enterobacteria, Pseudomonas aeruginosa, Acinetobacter baumannii and other non-fermenting Gram-negative bacilli]. Enfermedades Infecciosas Y Microbiología Clínica, 31(6), 402–9.
Gellatly, S. L., & Hancock, R. E. W. (2013). Pseudomonas aeruginosa: New insights into pathogenesis and host defenses. Pathogens and Disease, 67(3), 159–173. https://doi.org/10.1111/2049-632X.12033
Özen, A. I., & Ussery, D. W. (2012). Defining the Pseudomonas Genus: Where Do We Draw the Line with Azotobacter? Microbial Ecology. https://doi.org/10.1007/s00248-011-9914-8
Peix, A., Ramírez-Bahena, M.-H., & Velázquez, E. (2009). Historical evolution and current status of the taxonomy of genus Pseudomonas. Infection, Genetics and Evolution : Journal of Molecular Epidemiology and Evolutionary Genetics in Infectious Diseases, 9(6), 1132–1147.
Mac Aogáin, M., Kulah, C., Rijnsburger, M., Celebi, G., Savelkoul, P. H. M., O’Gara, F., & Mooij, M. J. (2012). Characterization of imipenem resistance mechanisms in Pseudomonas aeruginosa isolates from Turkey. Clinical Microbiology and Infection : The Official Publication of the European Society of Clinical Microbiology and Infectious Diseases, 18(7), E262-265.
Von Bodman, S. B., Willey, J. M., & Diggle, S. P. (2008). Cell-cell communication in bacteria: United we stand. In Journal of Bacteriology(Vol. 190, pp. 4377–4391). https://doi.org/10.1128/JB.00486-08
Kung, V. L., Ozer, E. A., & Hauser, A. R. (2010). The accessory genome of Pseudomonas aeruginosa. Microbiology and Molecular Biology Reviews : MMBR, 74(4), 621–41. https://doi.org/10.1128/MMBR.00027-10
El Solh, A. A., & Alhajhusain, A. (2009). Update on the treatment of Pseudomonas aeruginosa pneumonia. Journal of Antimicrobial Chemotherapy. https://doi.org/10.1093/jac/dkp201
Kung, V. L., Ozer, E. A., & Hauser, A. R. (2010). The accessory genome of Pseudomonas aeruginosa. Microbiology and Molecular Biology Reviews : MMBR, 74(4), 621–41. https://doi.org/10.1128/MMBR.00027-10
Høiby, N. (2011). Recent advances in the treatment of Pseudomonas aeruginosa infections in cystic fibrosis. BMC Medicine, 9, 32. https://doi.org/10.1186/1741-7015-9-32.
Williams, B. J., Dehnbostel, J., & Blackwell, T. S. (2010). Pseudomonas aeruginosa: Host defence in lung diseases. Respirology. https://doi.org/10.1111/j.1440-1843.2010.01819.x
Wei, Q., & Ma, L. Z. (2013). Biofilm matrix and its regulation in Pseudomonas aeruginosa. International Journal of Molecular Sciences. https://doi.org/10.3390/ijms141020983
Cooper, M., Tavankar, G. R., & Williams, H. D. (2003). Regulation of expression of the cyanide-insensitive terminal oxidase in Pseudomonas aeruginosa. Microbiology. https://doi.org/10.1099/mic.0.26017-0
Ubonchonlakate, K., Sikong, L., & Saito, F. (2012). Photocatalytic disinfection of P.aeruginosa bacterial Ag-doped TiO 2 film. In Procedia Engineering (Vol. 32, pp. 656–662). https://doi.org/10.1016/j.proeng.2012.01.1323
Patrick, R. M., & Baron, E. J. (2013). Manual of Clinical Microbiology. Journal of Chemical Information and Modeling (Vol. 1). https://doi.org/10.1017/CBO9781107415324.004
Otter, J. A., Vickery, K., Walker, J. T., deLancey Pulcini, E., Stoodley, P., Goldenberg, S. D., … Edgeworth, J. D. (2015). Surface-attached cells, biofilms and biocide susceptibility: Implications for hospital cleaning anddisinfection. Journal of Hospital Infection. https://doi.org/10.1016/j.jhin.2014.09.008
Gebel, J., Exner, M., French, G., Chartier, Y., Christiansen, B., Gemein, S, Sonntag, H.-G. (2013). The role of surface disinfection in infection prevention. GMS Hygiene and Infection Control, 8(1),
Krogulski, A. (2008). [Hospitals location and indoor air microbiological quality]. Roczniki Panstwowego Zakladu Higieny, 59(1), 97–102. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/18666627
Biccard, B. M., & Rodseth, R. N. (2011). Utility of clinical risk predictors for preoperative cardiovascular risk prediction. British Journal of Anaesthesia. https://doi.org/10.1093/bja/aer194
Vincent, C, Taylor-Adams, S, Champan, J, Hewett, D, Prior, S Strange, P, Tizzard, A. (2000). How to investigate and analyse clinical incidents: Clinical Risk Unit and Association of Litigation and Risk Management protocol. BMJ, 320(7237), 777–781.
Schechner, V., Nobre, V., Kaye, K. S., Leshno, M., Giladi, M., Rohner, P. Carmeli, Y. (2009). Gram-negative bacteremia upon hospital admission: when should Pseudomonas aeruginosa be suspected? Clinical Infectious Diseases : An Official Publication of the Infectious Diseases Society of
America, 48(5), 580–6. https://doi.org/10.1086/596709 Irazoqui, J. E., Troemel, E. R., Feinbaum, R. L., Luhachack, L. G., Cezairliyan, B. O., & Ausubel, F. M. (2010). Distinct pathogenesis and host responses during infection of C. elegans by P. aeruginosa and S. aureus. PLoS Pathogens, 6(7), 1–24. https://doi.org/10.1371/journal.ppat.1000982
Lanini, S., D’Arezzo, S., Puro, V., Martini, L., Imperi, F., Piselli, P., … Ippolito, G. (2011). Molecular epidemiology of a Pseudomonas aeruginosahospital outbreak driven by a contaminated disinfectant-soap dispenser. PLoS ONE, 6(2). https://doi.org/10.1371/journal.pone.0017064
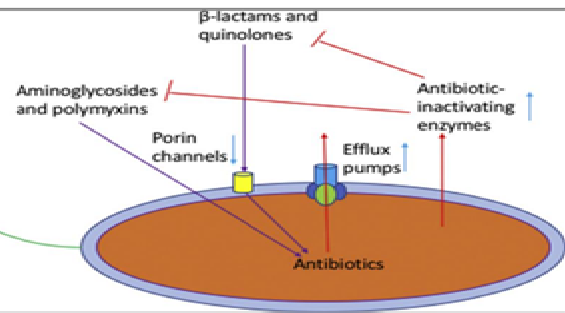
Lister, P. D., Wolter, D. J., & Hanson, N. D. (2009). Antibacterial-resistant Pseudomonas aeruginosa: Clinical impact and complex regulation of chromosomally encoded resistance mechanisms. Clinical Microbiology Reviews. https://doi.org/10.1128/CMR.00040-09
Miyata, S., Casey, M., Frank, D. W., Ausubel, F. M., & Drenkard, E. (2003). Use of the Galleria mellonella caterpillar as a model host to study the role of the type III secretion system in Pseudomonas aeruginosa pathogenesis. Infection and Immunity, 71(5), 2404–2413. https://doi.org/10.1128/IAI.71.5.2404-2413.2003
Karatuna, O., & Yagci, A. (2010). Analysis of quorum sensing-dependent virulence factor production and its relationship with antimicrobial susceptibility in Pseudomonas aeruginosa respiratory isolates. Clinical Microbiology and Infection, 16(12), 1770–1775. https://doi.org/10.1111/j.1469-0691.2010.03177.x
Morrison, a J., & Wenzel, R. P. (2015). Epidemiology of infections due to Pseudomonas aeruginosa. Reviews of Infectious Diseases, 6 Suppl 3, S627–S642. https://doi.org/10.1093/clinids/6.Supplement_3.S627
N Khardori. (2014). Future of diagnostic microbiology. Indian Journal of Medical Microbiology, 32(4), 371–377. https://doi.org/10.4103/0255-0857.142233
Berthelot, P., Grattard, F., Mallaval, F. O., Ros, a, Lucht, F., & Pozzetto, B. (2005). [Epidemiology of nosocomial infections due to Pseudomonas aeruginosa, Burkholderia cepacia and Stenotrophomonas maltophilia]. Pathologie-Biologie, 53(6), 341–8. https://doi.org/10.1016/j.patbio.2004.09.006
Marra, A.R., Bar, K., Bearman, G.M.L., Wenzel, R.P. and Edmond, M.B. 2006. Systemic inflammatory response syndrome in adult patients with nosocomial bloodstream infection due to Pseudomonas aeruginosa. Journal of Infection, 53 (1), pp.30-35.
Wright, G.D. 2005. Bacterial resistance to antibiotics: Enzymatic degradation and modification. Advanced Drug Delivery Reviews, 57 (10), pp.1451-1470.
Wu, S.J., Chan, A. and Kado, C.I. 2004. Detection of PCR amplicons from bacterial pathogens using microsphere agglutination. Journal of Microbiological Methods, 56 (3), pp.395-400.
Hawkins, C., Harper, D., Burch, D., Änggård, E. and Soothill, J. 2010. Topical treatment of Pseudomonas aeruginosa otitis of dogs with a bacteriophage mixture: A before/after clinical trial. Veterinary Microbiology, 146 (3-4), pp.309-313.
Authors
Copyright (c) 2024 https://creativecommons.org/licenses/by/4.0/

This work is licensed under a Creative Commons Attribution 4.0 International License.