Thrush Candidiasis: Classification, Chronic Hyperplastic Candidiasis, Systemic Immunocompromise, and Nutritional Deficiencies
Abstract
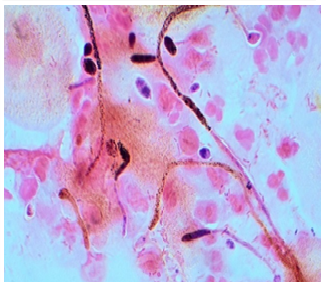
Thrush candidiasis, also known as oral candidiasis, is occurs in the mouth. This means that oral candidiasis is a mycosis (fungal/yeast infection) of the species of Candida on the mucous membranes of the mouth. Is an opportunistic infection of the oral cavity?
Aims of the study: - Studying candidia and its types, studying candidiasis, its types and divisions, and diagnosing a disease (candidiasis) in the mouth in children.
Methods: During the period between September 2021 and May 2022. In this study we have revised and reviewed most previous studies conducted on Candidiasis especially, Thrush and the method of isolation of candida species from oral cavity.
Result: According to statistics conducted by a number of researchers over the course of several years, and we studied them, we found several types of Candida that cause oral candida in children (C. albicans, C. tropicalis, C. glabrata, C. krusei .... etc). The rates of infection with C. albicans for 15 samples isolated from the mouth were (52%, 90%, 46%, 58.8%, 50%, 63%, 80%, 60.2%, 65%, 75%, 80. 7%, 69.35%, 61.5%, 43.7%) was the highest injury. While C. pseudotropicalis was found in two samples (1.8%, 4.6%) out of 15 samples, it can be considered the least infected.
Full text article
References
James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Philadelphia: Saunders Elsevier. p. 308. ISBN 978-0-7216-2921-6. OCLC 62736861.
Epstein JB. Antifungal therapy in oropharyngeal mycotic infections. Oral Surg Oral Med Oral Pathol 1990;69:32–41.
Guida RA. Candidiasis of the oropharynx and oesophagus. Ear NoseThroat J 1988;67:832–40.
Ghannoum MA, Radwan SS. Candida adherence to epithelial cells. Boca Raton, FL: CRC Press, 1990.
Abu-Elteen KH, Abu-Alteen RM. The prevalence of candida albicans populations in the mouths of complete denture wearers. New Microbiol 1998;21:41–8.
Arendorf TM, Walker DM. The prevalence and intra-oral distribution of Candida albicans in man. Arch Oral Biol 1980;25:1–10.
Holbrook WP, Hjorleifsdottir DV. Occurrence of oral Candida albicans and other yeast-like fungi in edentulous patients in geriatric units in Iceland. Gerodontics 1986;2;153–6.
Rodu B, Carpenter JT, Jones MR. The pathogenesis and clinical significance of cytologically detectable oral candida in acute leukaemia. Cancer 1988;62:2042–6.
Höfs, S.; Mogavero, S.; Hube, B. Interaction of Candida albicans with host cells: Virulence factors, host defense, escape strategies and the microbiota. J. Microbiol. 2016, 53, 149–169. [CrossRef]
Mayer, F.L.;Wilson, D.; Hube, B. Candida albicans pathogenecity mechanisms. Virulence 2013, 4, 119–128.[CrossRef]
Williams, D.; Lewis, M. Pathogenesis and treatment of oral candidosis. J. Oral Microbiol. 2011, 3. [CrossRef][PubMed]
Naglik, J.R.; Moyes, D.L.; Waächtler, B.; Hube, B. Candida albicans interactions with epithelial cells andmucosal immunity. Microbes Infect. 2011, 13, 963–976. [CrossRef][PubMed]
Manolakaki, D.; Velmahos, G.; Kourkoumpetis, T.; Chang, Y.; Alam, H. B.; De Moya, M. M.; Mylonakis, E. (2010). "Candida infection and colonization among trauma patients". Virulence. 1 (5): 367–75. doi:10.4161/viru.1.5.12796. PMID 21178472.
Kourkoumpetis TK, Velmahos GC, Ziakas PD, Tampakakis E, Manolakaki D, Coleman JJ, Mylonakis E (2011). "The effect of cumulative length of hospital stay on the antifungal resistance of Candida strains isolated from critically ill surgical patients". Mycopathologia. 171 (2): 85–91. doi:10.1007/s11046-010-9369-3. PMC 4093797. PMID 20927595.
Fugelsang, K.; Edwards, C. (2010). Wine Microbiology (2nd ed.). Springer. pp. 3–28. ISBN 978-0387333496.
Spanakis EK, Kourkoumpetis TK, Livanis G, Peleg AY, Mylonakis E (2010). "Statin therapy and decreased incidence of positive Candida cultures among patients with type 2 diabetes mellitus undergoing gastrointestinal surgery". Mayo Clin. Proc. 85 (12): 1073–9. doi:10.4065/mcp.2010.0447. PMC 2996154. PMID 21123633.
Nguyen NH, Suh SO, Blackwell M (2007). "Five novel Candida species in insect-associated yeast clades isolated from Neuroptera and other insects". Mycologia. 99 (6): 842–858. doi:10.3852/mycologia.99.6.842. PMID 18333508.
Suh SO, Nguyen NH, Blackwell M (2008). "Yeasts isolated from plant-associated beetles and other insects: seven novel Candida species near Candida albicans". FEMS Yeast Res.
8 (1): 88–102. doi:10.1111/j.1567-1364.2007.00320.x. PMID 17986254.
Steckelberg, James M. (2012-09-18). "Male yeast infection: Can I get it from my girlfriend?". Mayo Clinic. Retrieved 2014-03-23.
Gow, Neil A. R.; Yadav, Bhawna (2017). "Microbe Profile: Candida albicans: a shape-changing, opportunistic pathogenic fungus of humans". Microbiology. 163 (8): 1145–1147. doi:10.1099/mic.0.000499. PMID 28809155.
Pfaller, M. A.; Diekema, D. J.; Colombo, A. L.; Kibbler, C.; Ng, K. P.; Gibbs, D. L.; Newell, V. A. (2006). "Candida rugosa, an emerging fungal pathogen with resistance to azoles: geographic and temporal trends from the ARTEMIS DISK antifungal surveillance program". J. Clin. Microbiol. 44 (10): 3578–82. doi:10.1128/JCM.00863-06. PMC 1594768. PMID 17021085.
Spivak, Emily S.; Hanson, Kimberly E. (2017). "Candida auris: an Emerging Fungal Pathogen". Journal of Clinical Microbiology. 56 (2). doi:10.1128/JCM.01588-17. PMC 5786713. PMID 29167291.
Antifungal chemotherapy in patients with acquired immuno deficiency syndrome. British Society for Antimicrobial Chemotherapy Working Party. Lancet, 1992, 340(8820), 648-51.
Greenspan, D.; John, S.G. HIV-related oral disease. Lancet, 1996, 348, 729-734.
Smeekens, S.P.; Ng, A.; Kumar, V.; Johnson, M.D.; Plantinga, T.S.; van Diemen, C.; Arts, P.; Verwiel, E.T.; Gresnigt, M.S.; Fransen, K.; van Sommeren, S.; Oosting, M.; Cheng, S.C.; Joosten,
L.A.; Hoischen, A.; Kullberg, B.J.; Scott, W.K.; Perfect, J.R.; van der Meer, J.W.; Wijmenga, C.; Netea, M.G.; Xavier, R.J.
Functional genomics identifies type-I interferon pathway as central for host defense against C. albicans. Nat. Commun., 2013, 4, 1342.
Millsop, J.W.; Faze, L.N. Oral candidiasis. Clin. Dermatol. 2016, 34, 487–494. [CrossRef] [PubMed]
Hellstein, J.W.; Marek, C.L. Candidiasis: Red and white manifestations in the oral cavity. Head Neck Pathol.2019, 13, 25 32.
Lewis, M.A.O.;Williams, D.W. Diagnosis and management of oral candidosis. Br. Dent. J. 2017, 223, 675–681.
Bakri, M.M.; Hussaini, M.H.; Holmes, R.A.; Cannon, D.R.; Rich, M.A. Revisiting the association between candidal infection and carcinoma, particularly oral squamous cell carcinoma. J. Oral Microbiol. 2010, 2.
Williams, D.; Lewis, M. Pathogenesis and treatment of oral candidosis. J. Oral Microbiol. 2011, 3.
Sroussi, H.Y.; Epstein, J.B.; Bensadoun, R.J.; Saunders, D.P.; Lalla, R.V.; Migliorati, C.A.; Heaivilin, N.;Zumsteg, Z.S. Common oral complications of head and neck cancer radiation therapy: Mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017, 6, 2918–2931.
Khan, S.A.; Fidel, P., Jr.; Al Thunayyan, A.; Meiller, T.; Jabra-Rizk, M.A. Impaired histatin-5 level and salivary antimicrobial activity against C. albicans in HIV-infected individuals. J. AIDS Clin. Res. 2013, 4, 1000193.
Iinuma, T.; Arai, Y.; Abe, Y.; Takayama, M.; Fukumoto, M.; Fukui, Y.; Iwase, T.; Takebayashi, T.; Hirose, N.; Gionhaku, N.; et al. Denture wearing during sleep doubles the risk of pneumonia in the very elderly. J. Dent. Res. 2015, 94, 28S–36S.
Schaller, M.; Borelli, C.; Korting, H.C.; Hube, B. Hydrolytic enzymes as virulence factors of Candida albicans.Mycoses 2005, 48, 365–377.
Mun, M.; Yap, T.; Alnuaimi, A.D.; Adams, G.G.; McCullough, M.J. Oral candidal carriage in asymptomatic patients. Aust. Dent. J. 2016, 61, 190–195.
Manfredi, M.P.L.; Giovati, L.; Alnuaimi, A.; McCullough, M.J. Oral and Maxillofacial Fungal Infections.In Contemporary Oral Medicine; Farah, C., Balasubramaniam, R., McCullough, M., Eds.; Springer: Berlin/Heidelberg, Germany, 2018.
Johnson, D.; Yeh, C.K.; Dodds, M.W. E ect of donor age on the concentartions of histatins in human parotid and submandibular/sublingual saliva. Arch. Oral Biol. 2000, 45, 731–740.
Farah, C.S.; Lynch, N.; McCullough, M.J. Oral fungal infections: An update for the general practitioner. Aust. Dent. J. 2010, 5, 48–54.
Samaranayake, L.P.; Keung Leung,W.; Jin, L. Oral mucosal fungal infections. Periodontology 2000 2009, 49, 39–59.
Moulias R. Clinical manifestations of candidosis in the older adult. Revue de Geriatrie. 2002;49:1741-2
CDC: “Candidiasis,” “Oropharyngeal/Esophageal Candidiasis,” “Genital/vulvovaginal candidiasis (VVC),” “Invasive Candidiasis.”
HealthyChildren.org: “Thrush and Other Candida Infections, “Diaper Rash”https://www.webmd.com/skin-problems-and treatments/guide/what-is-candidiasis-yeast-infection.”
American Congress of Obstetricians and Gynecologists: “Vaginitis.” https://www.webmd.com/skin-problems-and-treatments/guide/what-is-candidiasis-yeast-infection .
WomensHealth.gov: “Vaginal Yeast Infection.” https://www.webmd.com/skin-problems-and-treatments/guide/what-is-candidiasis-yeast-infection .
National Health Service (U.K.): “Oral Thrush in Adults.” https://www.webmd.com/skin-problems-and-treatments/guide/what-is-candidiasis-yeast-infection .
Authors
Copyright (c) 2024 https://creativecommons.org/licenses/by/4.0/

This work is licensed under a Creative Commons Attribution 4.0 International License.